Once you understand the signs and symptoms that patients may experience with idiopathicThe term idiopathic is used when there is no detectable reason for something. Click the term to read more intracranial hypertension (IIH), familiarizing yourself with the diagnostic criteria is helpful in the evaluation of a suspected patient.
Known as the modified Dandy criteriaCriteria used for diagnosing patients with IIH. Click the term to read more, the diagnostic criteria for IIH was revised in 1985, from its original version in the 1930s. Four fundamental features are required to establish the diagnosis of IIH:
- Symptoms consistent with increased intracranial pressure: headaches, vomiting, and nausea. Visual signs and symptoms such as blurriness, transient obscurations of vision, and papilledemaSwelling of the optic nerve that carries visual signals from the eye to the brain. Click the term to read more.
- Normal neurological exam with the exception of unilateral or bilateral cranial VI nerve paresis.
- Elevated opening pressure on lumbar punctureA procedure where a needle is placed in the lower part of the spine (the lumbar spine) to access cerebrospinal fluid. Click the term to read more (greater than 250 mm) and normal analysis of cerebrospinal fluidFluid that is made by specialized cells in the ventricles of the brain. Click the term to read more.
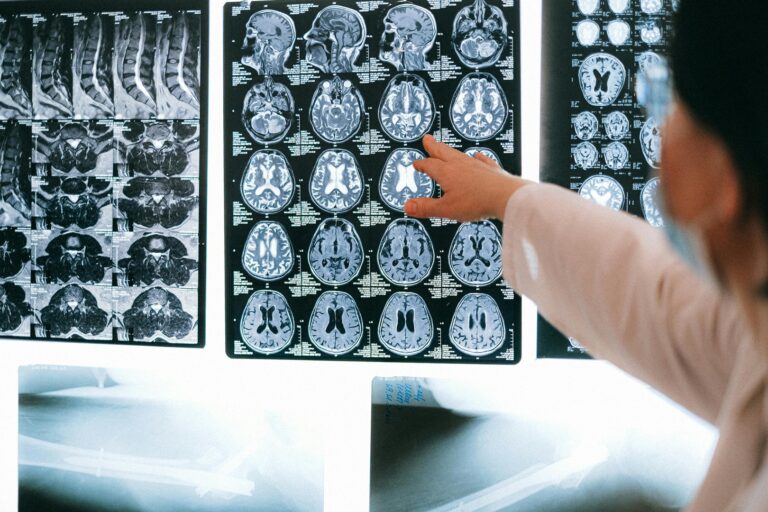
- Normal imaging of the brain1
Increased intracranial pressure can manifest in an array of symptoms from mild to severe. Headache is the most common complaint in one with IIH. This disabling symptom is nonspecific, highly subjective and conversely, patients without headache may have increased intracranial pressure. Other common complaints associated with an increased intracranial pressure are: nausea, vomiting, and visual complaints. A complete neurological exam is imperative to formulate a differential diagnosis.
The most common visual disturbance is blurring peripheral vision, due to the peripheral compression of the optic nerve. Transient obscurations of vision occur when a patient experiences spots or blurriness with a change in position, such as bending down to pick up an object. This occurs as elevated intracranial pressure is temporarily transferred to the optic disc. Papilledema – swelling of the optic nerve that carries visual signals from the eye to the brain – is not a requisite for diagnosis. Papilledema can be suspected by history alone as swelling of the optic nerve persists, vision worsens, and can progress to blindness, which can be permanent. The ability to see papilledema can be challenging and may need a specialist (such as a neuro-ophthalmologistMedical doctor who specializes in neurological conditions that affect vision. They can diagnose and treat conditions related to the optic nerve. Click the term to read more) to appreciate. Peripheral vision blurriness progressing to blindness is an emergency requiring immediate lumbar puncture and transfer to a facility in which specialty services can be provided.
A lumbar puncture is a minor diagnostic procedure that has associated complications that range from a more common, less severe risk such as headache to much more rare, but more serious risks such as meningitis. With proper technique and thorough consent for this procedure, these complications can be minimized. Ideally, the patient should be positioned in lateral decubitus, as that position minimizes a falsely elevated opening pressure. During a lumbar puncture, if the patient is in an upright position, valsalvas or coughs, it can falsely elevate the opening pressure measurement. A reading of greater than 250 mm is considered elevated.
It is recommended that at least 10 mL of CSFFluid that is made by specialized cells in the ventricles of the brain. Click the term to read more be withdrawn for a full analysis to be conducted. Specific testing of cerebrospinal fluid can include: microbiology, biochemistry, xanthochromia, oligoclonal bands, cytology, cytospin, viral PCR, angiotensin-converting enzyme, and lactate. Each component must result in a normal finding or another diagnosis should be investigated 2.