In this article we summarize a study that was published in the medical journal, Neurosurgery Practice this month. The lead author is Dr. Charles Matouk who is a NeurosurgeonMedical doctor who diagnoses and treats surgical issues related to the brain, spine, and nervous system. Click the term to read more, Professor and Vice Chair (Clinical Affairs) and Chief of Neurovascular Surgery at Yale Department of Neurosurgery.
During our chat session in September, a large interest was on the topic of shunts and IIH. We discussed at length the difference between a lumboperitoneal shuntA procedure that prevents the accumulation of excess cerebrospinal fluid in the brain. Click the term to read more (LPSA procedure that prevents the accumulation of excess cerebrospinal fluid in the brain. Click the term to read more) and a ventriculoperitoneal shuntA procedure undertaken to prevent accumulation of excess cerebrospinal fluid in the brain Click the term to read more (VPSA procedure undertaken to prevent accumulation of excess cerebrospinal fluid in the brain Click the term to read more). This article examines a third shuntA hollow tube that can be surgically placed in the sinus to help drain cerebrospinal fluid. Click the term to read more option called a lumbocaval shunt (LCS).
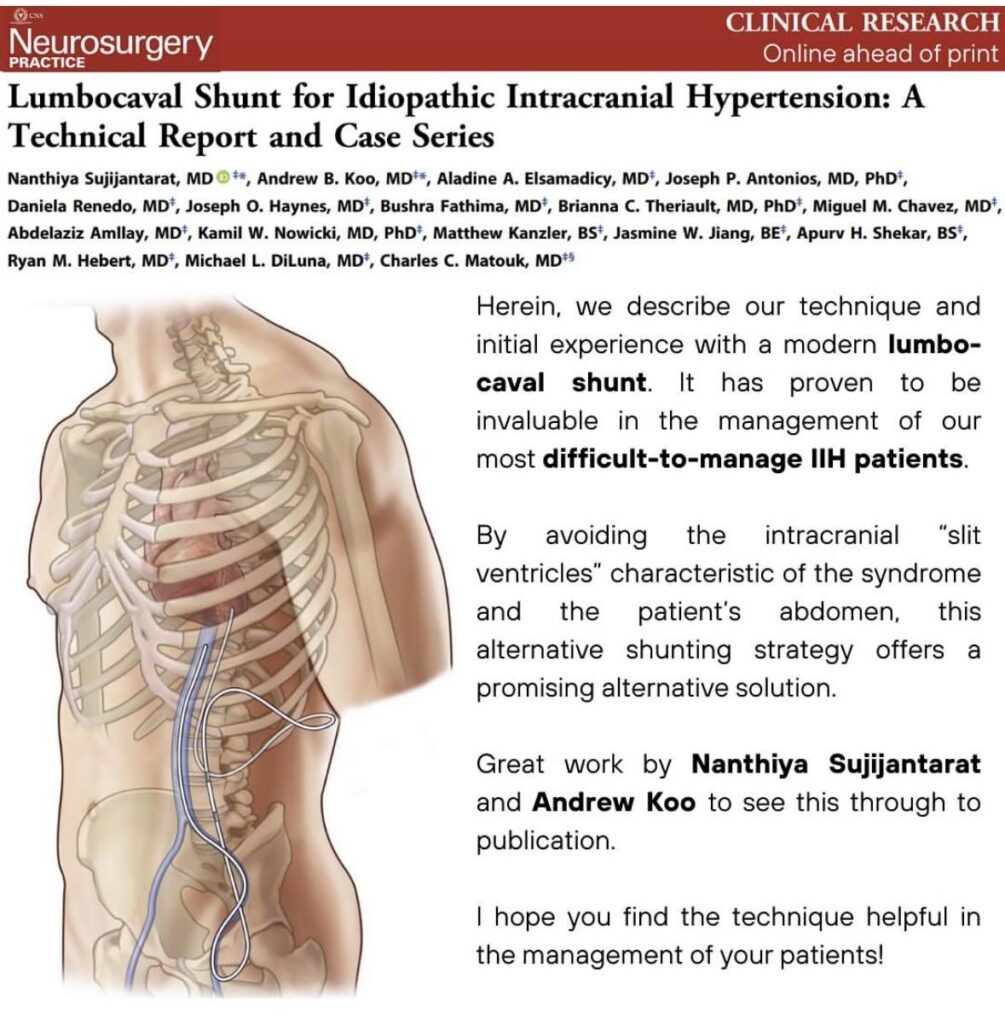
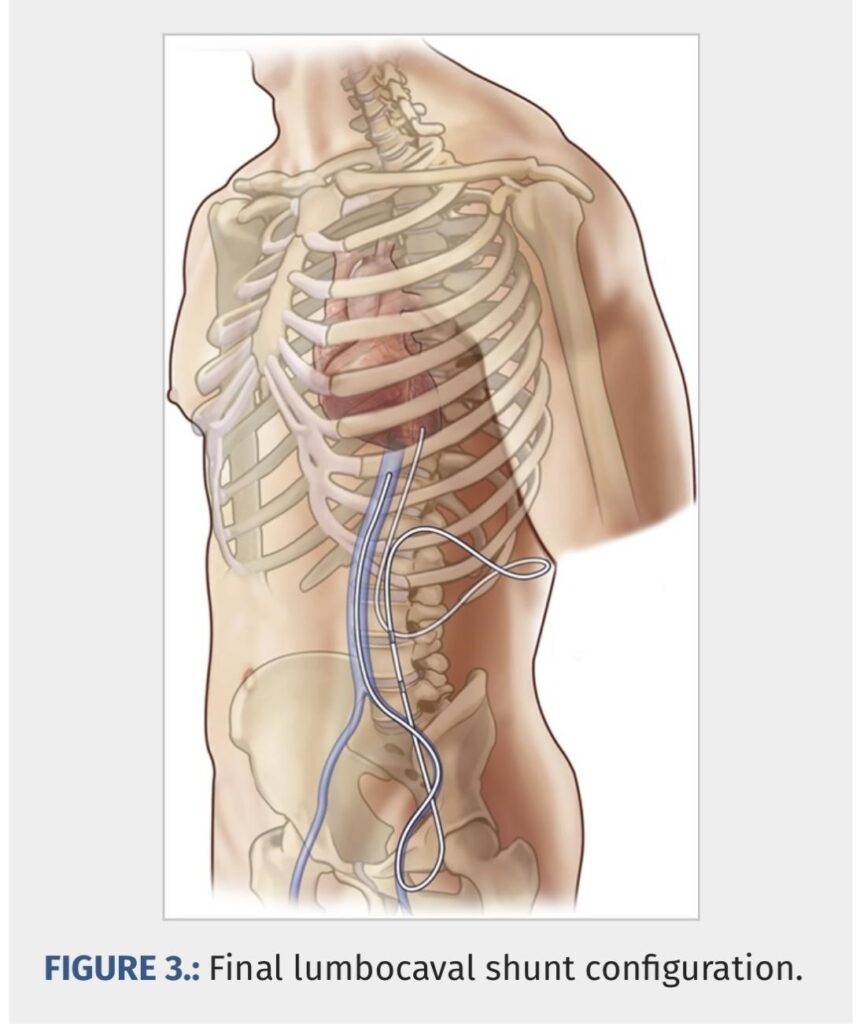
A lumbocaval shunt (LCS) is the placement of a catheter in the lumbar area of the back to drain cerebrospinal fluidFluid that is made by specialized cells in the ventricles of the brain. Click the term to read more (CSFFluid that is made by specialized cells in the ventricles of the brain. Click the term to read more) into the inferior vena cava of the heart. In this procedure the shunt is accessed typically between the L2 and L3 interspinous space and placed in the subarachnoid space. The other half of the shunt is placed into the heart typically into the inferior vena cava. The heart will then disperse the CSF to be resorbed by the body.
In this study, the Neurosurgical Department at Yale retrospectively reviewed 6 women diagnosed with IIH using the modified Dandy criteriaCriteria used for diagnosing patients with IIH. Click the term to read more. These women failed medical management and had a previous shunt placement or revision.
Here is an excerpt from the article:
“In our series, all patients had slit ventricles, making intracranial shunt placement more technically challenging. Moreover, ventricular collapse around the shunt catheter may be an important contributor to shunt failure in this difficult-to-manage population.17Placement of the distal shunt catheter outside of the peritoneal space may also be advantageous. Physiologically, intraabdominal pressure is higher in obese patients.18 Because obesity is a common comorbidity associated with IIH, a diminished gradient between the intracranial pressure and intra-abdominal pressure may reduce the effectiveness of CSF drainage.19,20 This insight remains speculative because much is lacking in our understanding of the pathophysiology of IIH. Longer follow-up in a larger sample set is needed to determine where LCS fits into the treatment paradigm of IIH.”
Some important factors were learned from this study:
- An LP or LC shunt is preferred over a VP shunt when slit-like ventricles are seen.
- The lumbar end of the shunt is placed higher than usual to allow space for subsequent lumbar punctures, common in the management of IIH.
- A drawback of a LCS is the inability to interrogate it to determine failure or infection.
- Due to the small sample size and short-term follow up of this study, more information will need to be obtained in future studies to determine how effective an LCS can be the management of those with IIH.
Thank you for Dr. Charles Matouk and his team for furthering research in the field of IIH. You can follow Dr. Matouk on his instagram or see him as a patient.



